The New Ultrasound and Magnetic Resonance Imaging Qualification Tools for Metabolic Liver Disease: Why and How Should Radiologists Use Them?
Overview
An overview of liver disease caused by metabolism
Imaging’s significance in diagnosis and treatment
Developments in qualifying tools for magnetic resonance imaging (MRI) and ultrasound (US)
Comprehending Liver Metabolic Disease
Types of metabolic liver disorders and their definitions
Common ailments (Hemochromatosis, Wilson’s disease, NASH, and NAFLD)
Imaging’s function in evaluating liver health
Conventional Imaging Methods for Liver Disorders: Making a diagnosis
The gold standard, yet invasive, liver biopsy
The limits of conventional ultrasound
The function of CT scans in liver evaluation
Developments in Metabolic Liver Disease Ultrasonography
Elastography by shear waves (SWE)
CEUS, or contrast-enhanced ultrasonography
Using the controlled attenuation parameter (CAP) to quantify fat
Advances in Magnetic Resonance Imaging for Liver Evaluation
Elastography using magnetic resonance (MRE)
T2* mapping of proton density fat fraction (PDFF) for evaluating iron overload
Why Do Radiologists Need to Verify These New Instruments?
Reliability and accuracy in contrast to biopsy
Cutting back on invasive treatments
Benefits of early disease identification and staging
How to Verify MRI and Ultrasound Instruments for Clinical Applications
Comparative research and clinical trials
Putting in place uniform procedures
Radiologists’ education and certification
Implementing Advanced Imaging Tools Presents Difficulties
Issues with accessibility and cost
Specialized training is required.
Variability in the interpretation and imaging results
Applications in the Real World and Case Studies
Achievements in diagnosing NAFLD/NASH
influence on patient outcomes and treatment choices
Imaging’s Future in Metabolic Liver Disease
Machine learning and artificial intelligence (AI) in imaging
Electronic health record (EHR) integration
Possibility of real-time, non-invasive monitoring
In conclusion
An overview of the advantages of emerging imaging technologies
Urging radiologists to embrace and verify these technologies
FAQs
What is the difference between modern and old ultrasound techniques?
Why is MRI a superior choice for evaluating liver disease?
Do many people have access to these imaging tools?
How may radiologists receive instruction in these novel methods?
How will non-invasive liver disease diagnosis develop in the future?
 Overview
Overview
Non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH) are two metabolic liver diseases that are becoming more and more of a global health problem. Timely action depends on accurate diagnosis and staging, and imaging is essential to both processes. Although liver biopsies have historically been considered the gold standard, their invasiveness and related hazards have sparked a search for less invasive options.
Without requiring a biopsy, new magnetic resonance imaging (MRI) and ultrasound (US) technologies present intriguing alternatives for assessing metabolic liver disease. These cutting-edge imaging methods offer iron overload detection, fibrosis staging, and quantitative liver fat evaluation. However, radiologists need to confirm the accuracy, dependability, and clinical value of these techniques before they become commonplace.
In order to improve patient outcomes and manage liver disease as effectively as possible, this article examines the reasons why and methods by which radiologists should validate and incorporate these novel imaging modalities into their clinical workflow.
Comprehending Liver Metabolic Disease
A variety of illnesses affecting the liver as a result of metabolic imbalances are referred to as metabolic liver diseases. Among the most prevalent conditions are:
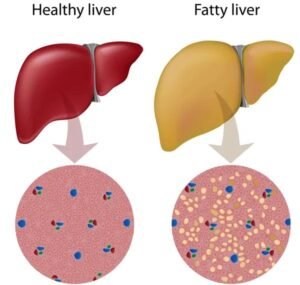
Excess fat buildup in the liver that is not connected to alcohol use is known as non-alcoholic fatty liver disease (NAFLD).
A more severe kind of NAFLD that involves inflammation and liver damage is called non-alcoholic steatohepatitis (NASH).
Hemochromatosis: A condition that causes the liver to accumulate too much iron.
Wilson’s disease: A hereditary disorder that causes the liver to accumulate copper.
If these disorders are not identified in time, they may develop into cirrhosis, fibrosis, and liver failure. Liver biopsies are less necessary because of imaging technology, which offers a non-invasive way to diagnose and track these conditions.
 Conventional Imaging Methods for Liver Disorders: Making a diagnosis
Conventional Imaging Methods for Liver Disorders: Making a diagnosis
Liver Biopsy: The Most Reliable Method
The main technique for identifying metabolic liver disorders for many years has been liver biopsy. Although it offers comprehensive histopathology data, it has a number of shortcomings:
invasive process that carries an infection and bleeding risk.
mistakes in sampling as a result of small tissue extraction.
High expenses and patient discomfort.
Traditional Ultrasonography and Its Drawbacks
Although it is frequently utilized for liver imaging, traditional ultrasonography (US) has drawbacks.
operator-dependent, which causes findings to vary.
limited capacity to distinguish between fibrosis and fatty liver.
CT scans to evaluate the liver
Although CT scans offer detailed imaging, they have limitations.
exposure to radiation, which makes it less suitable for regular observation.
less sensitive than MRI in terms of fat estimation.
Non-invasive imaging methods such as shear wave elastography (SWE), contrast-enhanced ultrasound (CEUS), and MRI-based approaches have advanced as a result of these constraints.
Developments in Metabolic Liver Disease Ultrasonography
Elastography using Shear Waves (SWE)
By measuring liver stiffness, SWE offers a trustworthy way to evaluate cirrhosis and fibrosis. Compared to conventional ultrasonography, it is superior because
Rather than subjective evaluations, it provides quantifiable measurements.
Because it is reproducible and non-invasive, fewer biopsies are required.
Contrast-Enhanced Ultrasound (CEUS): CEUS enhances vascular evaluation and liver lesion characterization. Advantages consist of:
improved identification of malignancies and liver fibrosis.
imagery in real time without being exposed to radiation.
Fat Quantification Using the Controlled Attenuation Parameter (CAP)
When combined with transient elastography, CAP offers a trustworthy way to measure liver fat. It is beneficial for:
diagnosing NAFLD and monitoring its course.
separating fibrosis from fatty liver without a biopsy.
Advances in Magnetic Resonance Imaging for Liver Evaluation
Elastography using Magnetic Resonance (MRE)
MRE is thought to be better than elastography based on ultrasound because:
It improves the stage of fibrosis by providing comprehensive maps of liver stiffness.
Obesity and other patient-related factors have less of an impact.
Fat Quantification Using Proton Density Fat Fraction (PDFF)
An MRI-based instrument called PDFF precisely measures the amount of liver fat, which makes it:
more accurate than fat-measuring techniques based on ultrasonography.
Perfect for tracking patients with NASH and NAFLD over time.
T2 Mapping for the Evaluation of Iron Overload
For the detection of iron overload in diseases such as hemochromatosis, this MRI method is essential. It is beneficial:
Examine the amount of iron deposited in liver tissue.
Provide guidance for iron-chelation therapy treatment choices.
Why Do Radiologists Need to Verify These New Instruments?
In order to use and validate these technologies, radiologists are essential since they:
Assure precision in contrast to conventional biopsy-based techniques.
Improve patient safety by reducing intrusive procedures.
Facilitate early disease detection to improve treatment results.
For these technologies to be widely used, they must be validated through studies and clinical trials.
How to Verify MRI and Ultrasound Equipment for Clinical Use
A systematic validation approach is required before radiologists can confidently incorporate new ultrasound (US) and magnetic resonance imaging (MRI) qualifying tools into their daily practice. These tools can be successfully validated in the following ways:
1. Performing Comparative Research and Clinical Trials
To compare the accuracy of new imaging methods to liver biopsy, the current gold standard, radiologists should take part in extensive clinical trials.
Sensitivity, specificity, and repeatability of results across various patient populations should be the main emphasis of studies.
Multi-center studies can guarantee that the technology is widely applicable and assist in removing bias.
2. Creating Uniform Imaging Procedures
Standardizing imaging practices is necessary for validation in order to guarantee uniformity across clinics and hospitals.
The European Association for the Study of the Liver (EASL) and the American College of Radiology (ACR) are two organizations that can assist in establishing consistent usage standards.
To lessen operator variability, protocols should cover patient placement, machine calibration, and interpretation standards.
3. Radiologists’ Education and Certification
Radiologists must complete specialized training and certification programs because these cutting-edge imaging techniques call for specific understanding.
The ability to understand elastography, PDFF, and other advanced imaging results can be enhanced through practical workshops, AI-assisted learning, and continuing medical education (CME) courses.
Radiologists who have earned certification from professional radiology societies are guaranteed to be qualified to make precise diagnoses.
By taking these actions, radiologists can make sure that newly developed US and MRI instruments are clinically sound and prepared for general use in the diagnosis of metabolic liver disease.
 Implementing Advanced Imaging Tools Presents Difficulties
Implementing Advanced Imaging Tools Presents Difficulties
Although there are many advantages to sophisticated imaging technology, adoption is not without difficulties.
1. Issues with Cost and Accessibility
Not all healthcare facilities may have access to high-end MRI scanners with MRE and PDFF capabilities due to their high cost.
These imaging modalities’ reimbursement rules are still being developed, which may affect patients’ ability to afford them.
It is still difficult to find qualified radiologists who are skilled in these methods in environments with limited resources.
2. Specialized Training Is Necessary
SWE, CEUS, and MRI-based methods necessitate further training than traditional ultrasound.
Inaccurate diagnosis could come from misinterpreting imaging results if one is not well educated.
AI-assisted interpretation and training initiatives can aid in closing the knowledge gap.
3. Variability in Imaging Outcomes
Dependency on the operator might result in variable measurements amongst clinicians, especially when using ultrasound-based procedures.
Consistency and reproducibility can be enhanced with the use of AI-assisted diagnostic tools and standardized imaging techniques.
Notwithstanding these obstacles, it is anticipated that ongoing policy changes and technology developments will make it easier for these imaging methods to be widely used in the years to come.
Applications in the Real World and Case Studies
1. Research on Non-Alcoholic Fatty Liver Disease (NAFLD) and NASH has demonstrated that MRI-PDFF is a better method for measuring liver fat content than ultrasound-based CAP.
As an alternative to liver biopsy, MRE has been successful in staging fibrosis.
These techniques are currently being used by radiologists at large medical facilities to track the course of the disease and the effectiveness of treatment in patients with non-alcoholic fatty liver disease.
2. Iron Overload and Hemochromatosis
Iron overload in patients with hereditary hemochromatosis* has been identified with the aid of MRI-based T2 mapping.
This method has improved patient outcomes and enabled earlier therapy initiation by taking the place of liver biopsy.
3. Using Contrast-Enhanced Ultrasound (CEUS) to Characterize Liver Lesions
For identifying liver tumors and differentiating between benign and malignant lesions, CEUS has been widely used.
Because CEUS doesn’t use radiation like CT and MRI do, it’s a safer option for repeated imaging.
These practical uses demonstrate how confirming and applying cutting-edge imaging methods can enhance patient care and diagnostic precision.
 Imaging’s Future in Metabolic Liver Disease
Imaging’s Future in Metabolic Liver Disease
1. Artificial Intelligence (AI) Integration in Imaging
AI is anticipated to be crucial in automating the staging of fibrosis and the quantification of liver fat.
By improving diagnostic accuracy and decreasing variability in image interpretation, AI-driven algorithms can help radiologists.
2. Non-Invasive Real-Time Monitoring
Non-invasive liver monitoring may become commonplace as wearable imaging technology and portable ultrasound equipment advance.
Patients with metabolic liver disease might be able to monitor their liver health in real time thanks to future developments.
3. Tailored Intervention Techniques
By forecasting the course of the disease, AI and advanced imaging tools will allow for individualized treatment approaches.
Imaging biomarkers can be used to guide lifestyle changes and early intervention for patients at risk of NASH progression.
By eliminating the need for invasive procedures, these advancements are anticipated to completely transform the way radiologists identify and treat metabolic liver disorders.
In conclusion
The diagnosis and monitoring of metabolic liver disorders are being revolutionized by new MRI and ultrasound qualification methods. These imaging methods enhance early diagnosis, patient safety, and treatment efficacy by offering precise, non-invasive substitutes for liver biopsies.
Radiologists must, however, concentrate on confirming these technologies’ dependability through training courses, clinical trials, and established procedures if they are to become commonplace. These developments have the potential to completely transform the treatment of metabolic liver disease, notwithstanding obstacles like expense, accessibility, and the requirement for specific training.
As radiology advances, embracing AI and real-time imaging solutions will significantly improve diagnostic capabilities, paving the way for improved patient care and tailored medication.
FAQ 1. What is the difference between new and old ultrasound techniques?
In contrast to standard grayscale ultrasonography, which is more subjective and operator-dependent, new ultrasound techniques like shear wave elastography (SWE) and contrast-enhanced ultrasound (CEUS) provide more accurate and quantitative evaluations.
2. Why is MRI a superior choice for evaluating liver disease?
For a thorough evaluation of the liver, MRI-based techniques like MRE, PDFF, and T2 mapping* are better than ultrasound because they offer extremely accurate assessments of liver stiffness, fat content, and iron overload.
3. How broadly accessible are these imaging tools?
Ultrasound elastography is becoming more widely available in standard clinical settings, whereas MRI-based methods are more frequently seen in tertiary facilities. Costs and training, however, continue to be obstacles in some areas.
4. How may radiologists receive instruction in these novel methods?
Professional associations such as the European Association for the Study of the Liver (EASL) and the Radiological Society of North America (RSNA) provide CME courses, practical workshops, and AI-assisted training modules for radiologists.
5. How will non-invasive liver disease diagnosis develop in the future?
AI integration, real-time monitoring, and customized treatment plans are the way of the future. They will lessen the need for intrusive biopsies and enable early liver disease detection and intervention.