Hepatocellular Carcinoma: Understanding, Prevention, and Treatment
Overview
With more than 80% of all liver cancer cases occurring globally, hepatocellular carcinoma (HCC) is the most prevalent form of primary liver cancer. Understanding the causes, symptoms, diagnostic procedures, and available treatments for HCC is crucial due to its substantial impact, particularly in areas where hepatitis infections are common. We’ll go into the intricacies of HCC in this piece and examine contemporary approaches to treating and preventing this powerful illness.

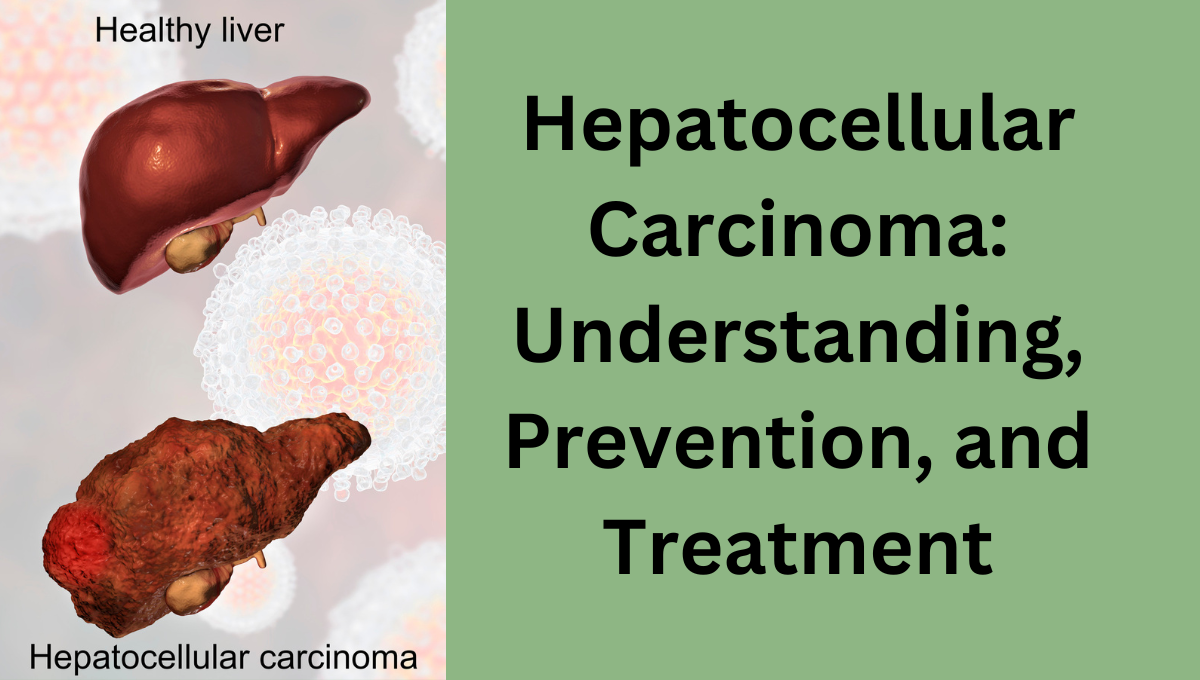
Hepatocellular Carcinoma: What is it?
Hepatocytes, the main liver cells, are the site of origin for hepatocellular carcinoma, a malignant tumor. HCC can rapidly impair general health since the liver is a key organ for the metabolism of poisons and the synthesis of vital proteins. Chronic inflammation, often triggered by heavy drinking, hepatitis B or C infections, or illnesses such as nonalcoholic fatty liver disease (NAFLD), typically manifests in the liver.
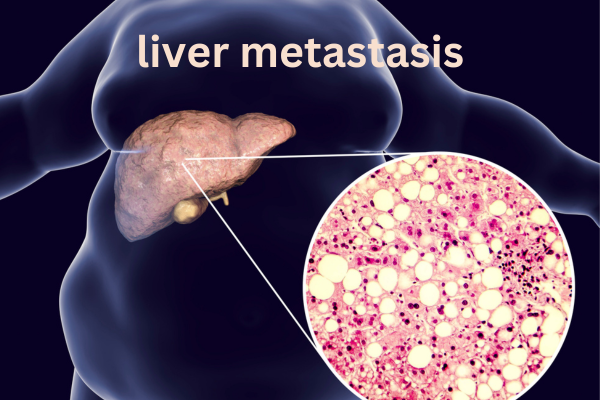
Comparing HCC with other liver cancers
Although HCC is the most common kind of liver cancer, angiosarcoma and intrahepatic cholangiocarcinoma are also possible. These tumors have different hepatic origins and call for different treatment modalities. The attention on HCC is due to its prevalence and correlation with common risk factors, such as liver cirrhosis and viral infections.
Hepatocellular carcinoma epidemiology
East Asia and sub-Saharan Africa have the greatest prevalence of HCC, making it a worldwide health concern. However, as NAFLD and hepatitis C infection rates rise, so does the prevalence of HCC in the US and Europe. Despite the significant influence of lifestyle choices and treatment accessibility on the disease’s spread and consequences, men, particularly those over 50, bear a disproportionate burden.
Risk Factors Affecting the Development of HCC
Early identification and preventive efforts can benefit from an understanding of the main risk factors:
Chronic Viral Hepatitis: Hepatitis B and C infections, the primary cause of the disease, account for up to 80% of cases of HCC worldwide.
Cirrhosis: Associated with alcohol misuse, viral hepatitis, or fatty liver disease, this severe scarring of liver tissue frequently precedes HCC.
NAFLD, also known as nonalcoholic fatty liver disease, is linked to obesity and metabolic syndrome and can lead to hepatic inflammation and HCC.
Abuse of Alcohol: Excessive alcohol use causes cirrhosis, which significantly increases the risk of liver cancer.
Exposure to Aflatoxin: Aflatoxin, a recognized carcinogen that raises the risk of HCC, is present in tainted grains and nuts.
Early hepatocellular carcinoma symptoms and signs
Missing early-stage HCC symptoms frequently leads to delayed diagnosis and a decreased survival rate. However, a few warning signs may indicate potential liver issues that require immediate attention:
Unexplained Weight Loss: One of the most frequent early signs of liver cancer is sudden, inadvertent weight loss.
Persistent Abdominal Pain: Discomfort or a feeling of fullness in the upper right abdomen may indicate liver problems.
Jaundice: Impaired liver function causes the skin and eyes to turn yellow.
Loss of appetite: Liver dysfunction may also be indicated by a lack of appetite, which is frequently accompanied by nausea.
Abdominal swelling: As liver function deteriorates, fluid buildup, or ascites, is a typical symptom.
Early detection of these signs can result in better results and a speedier intervention.
How does one make a diagnosis of hepatocellular carcinoma?
An accurate diagnosis is essential for effective treatment of HCC. Healthcare professionals use a range of techniques to identify and evaluate the stage of HCC:

1. Examinations of the blood
A blood test can reveal elevated levels of alpha-fetoprotein (AFP), a marker frequently linked to liver cancer. However, additional imaging studies are typically required because increased AFP levels are not unique to HCC.
2. Imaging Examinations
Imaging is essential to the diagnosis of HCC.
A common first-line method for identifying abnormal liver growths is ultrasound.
CT scans and MRIs, two precise imaging techniques, can determine the size, location, and spread of liver tumors.
Sometimes, doctors use PET scans to detect cancer that has spread to other organs.
3. The biopsy
If imaging and blood tests indicate liver cancer, a biopsy may confirm the diagnosis. During a biopsy, we remove a tiny sample of liver tissue and examine its contents for malignant cells.
4. HCC Staging Systems
The Barcelona Clinic Liver Cancer (BCLC) approach frequently stages HCC. To direct treatment, it evaluates variables such as liver function, tumor growth, and general health. Other systems include the Child-Pugh score, which focuses on liver function, and the TNM staging system, which assesses tumor features and dissemination.
Options for Hepatocellular Carcinoma Treatment
Tumor stage, liver function, and patient health are some of the variables that affect HCC treatment. Surgery and targeted therapy are two options that are appropriate for varying stages of the disease.
1. Resection via surgery.
If the cancer is localized and the liver is still working normally, the tumor may be surgically removed. Although resection may be curative, it is only appropriate for a tiny proportion of individuals who receive an early diagnosis.
2. Transplantation of the liver
If surgical removal of the tumor is not possible, a liver transplant may be an option. This treatment is effective for individuals with limited tumor spread, as it removes the entire diseased liver and replaces it with a healthy donor liver. However, it is a less accessible option due to transplant availability and stringent qualifying requirements.
3. Techniques for Ablation
Ablation kills cancer cells by injecting them with heat, ice, or chemicals. These minimally invasive techniques work well for small, early-stage cancers and are appropriate for patients who are unable to have surgery.
Radiofrequency ablation (RFA) uses heat to destroy cancer cells.
Cryoablation targets and freezes cancer cells at extremely low temperatures.
Percutaneous Ethanol Injection (PEI): This method involves injecting alcohol straight into the tumor to kill cells.
4. Focused Treatment
Targeted medications target particular chemicals found in cancer cells. Targeted treatments like lenvatinib and sorafenib help decrease the evolution of HCC, especially in more advanced instances. These medications can prolong survival and enhance quality of life even though they cannot cure HCC.

5. Immunotherapy
In order to combat cancer cells, immunotherapy stimulates the body’s immune system. Pembrolizumab and other checkpoint inhibitors have shown promise for certain HCC patients, particularly those with advanced, incurable malignancies. Although outcomes differ depending on patient characteristics, immunotherapy can increase survival rates.
6. Treatment with radiation
Radiation, especially stereotactic body radiation treatment (SBRT), precisely targets liver cancers. When surgery is not an option, people typically employ radiation, despite its potential serious side effects, especially in those with pre-existing liver problems.
7. The use of chemotherapy
Because of the liver’s metabolic function, traditional chemotherapy is less successful for HCC than for other malignancies. Chemoembolization, which injects chemotherapy straight into the liver, can nevertheless delay the growth of advanced tumors.
Hepatocellular Carcinoma Prevention
Prevention techniques are essential for lowering the prevalence of HCC, as they focus on modifiable risk factors.
1. Hepatitis B vaccination
When it comes to avoiding HCC, the hepatitis B vaccine is very successful. In high-risk areas, universal vaccination has significantly decreased the incidence of liver cancer in recent decades.
2. Hepatitis C screening
Early detection and treatment of hepatitis C infection can prevent cirrhosis and ultimately HCC. Because antiviral drugs have been so successful in curing hepatitis C, screening is crucial.
3. Controlling alcohol use.
Avoiding excessive alcohol use is crucial to preventing liver damage. Cutting back on alcohol consumption reduces the risk of cirrhosis and, in turn, HCC.
4. Keeping your weight in check.
Diabetes and obesity are major risk factors for NAFLD, which can develop into HCC. For liver health, a balanced diet, consistent exercise, and weight control are crucial.
5. Reducing Exposure to Aflatoxin
HCC risk can be decreased by avoiding foods that might contain aflatoxins, such as nuts and cereals that are not adequately stored. In many regions of the world, regulatory actions have also reduced exposure to aflatoxin.
Current studies and prospects for treating HCC
Because HCC is becoming more common, researchers are working to improve detection and treatment techniques.
1. The development of innovative, targeted therapies
In order to improve the efficacy for patients with advanced HCC, recent research is investigating next-generation targeted medicines intended to counteract resistance mechanisms in liver cancer cells.
2. Combination Therapy
Targeted medication and immunotherapy have demonstrated promise together, possibly producing synergistic benefits that can better regulate HCC growth than single-agent therapies.
3. Research on Biomarkers
Finding particular biomarkers for early HCC identification is still a crucial research topic. Biomarkers could greatly increase survival rates by enabling medical professionals to identify HCC in its early stages.
4. Tumor Genetic Profiling
Genomic advancements are enabling personalized therapeutic approaches. By customizing treatments to the distinct genetic composition of each patient’s tumor, genetic profiling enables physicians to maximize therapy results.
In conclusion
Hepatocellular carcinoma is a difficult and frequently violent cancer that affects people all over the world. The best way to lower the incidence of HCC is to prevent it through immunization, routine screenings, and healthy lifestyle choices. Improvements in immunotherapy, targeted treatments, and surgical methods are giving people with HCC fresh hope for better results. Despite the ongoing challenges, current research is making significant strides in the management, diagnosis, and therapy of this complex illness.
FAQs
1. What are hepatocellular carcinoma’s primary symptoms?
Abdominal pain, jaundice, appetite loss, weight loss, and edema are early signs of HCC. Regular screening for at-risk persons is essential since these symptoms frequently go undetected until the cancer has progressed.
2. What is the standard treatment for HCC?
Surgical excision, liver transplantation, ablation, targeted therapy, immunotherapy, and occasionally chemotherapy are among the possible treatments, depending on the stage of the cancer. We consider the patient’s liver function and general health when choosing an alternative.
3. Can altering one’s lifestyle lower the chance of getting HCC?
Indeed, altering one’s lifestyle to minimize alcohol intake, keep a healthy weight, and stay away from aflatoxins can lower the risk of HCC. Other crucial preventive strategies include routine hepatitis C testing and hepatitis B vaccination.
4. Does HCC run in families?
Although a family history of liver illness or hepatitis infection can raise an individual’s risk, HCC is not directly inherited. In certain situations, genetic profiling can assist in determining an individual’s susceptibility.
5. How do individuals with HCC fare?
Depending on the patient’s liver function and the stage of the cancer at diagnosis, the prognosis for HCC varies greatly. The best opportunity for effective treatment and higher survival rates is through early detection.