Comprehending Systemic Lupus Erythematosus Overlap Syndrome and Autoimmune Hepatitis
Overview
Comprehending Systemic Lupus Erythematosus Overlap Syndrome and Autoimmune Hepatitis When the body’s immune system unintentionally targets its own tissues, autoimmune disorders result. Sometimes people will have symptoms from two different autoimmune diseases at the same time. One example is the overlap between Systemic Lupus Erythematosus (SLE) and Autoimmune Hepatitis (AIH), an uncommon and complicated combination that presents particular difficulties for diagnosis and treatment.
The causes, symptoms, diagnosis, and treatment of this overlap syndrome are examined in this article.
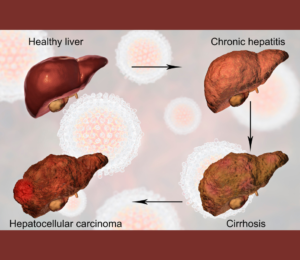
Autoimmune Hepatitis: What Is It? Liver inflammation is a hallmark of the chronic illness known as autoimmune hepatitis. If left unchecked, the immune system’s attack on the liver cells might result in cirrhosis and liver failure.
Important Characteristics of AIH: **Symptoms**: Joint pain, fatigue, jaundice, and stomach discomfort. – **Diagnosis**: Liver biopsy results and blood tests showing increased liver enzymes and autoantibodies. – **Treatment**: The illness is often managed with immunosuppressive drugs such azathioprine and corticosteroids.
Systemic Lupus Erythematosus: What is it?
Lupus systemic A complicated autoimmune condition, erythematosus can impact the skin, joints, kidneys, and neurological system, among other bodily systems. Extreme exhaustion and a “butterfly” rash across the cheeks are hallmarks of SLE.
Important Characteristics of SLE: **Symptoms**: joint pain, fever, exhaustion, rash, kidney problems, and neurological symptoms. –
**Diagnosis**: Clinical assessment and blood tests for antinuclear antibodies (ANA) and other particular autoantibodies.
**Treatment**: NSAIDs, immunosuppressants, and antimalarials such as hydroxychloroquine to control symptoms.
## AIH with SLE Overlap Syndrome A uncommon clinical overlap occurs when patients with AIH and SLE exhibit with characteristics of both diseases. Accurate diagnosis and efficient treatment depend on an understanding of this overlap.
### Risk factors and causes Although the precise processes causing overlap syndromes are not entirely understood, several environmental and genetic variables might be involved. In predisposed people, shared autoantigens and immune system pathways may cause both SLE and AIH.
**Genetic Predisposition**: Certain HLA genotypes are associated with SLE and AIH, indicating that genetic susceptibility plays a role in both disorders. **Environmental Triggers**: Stress, drugs, and infections can all cause an autoimmune reaction that can result in the development of an illness.
Typical Signs Individuals with SLE overlap syndrome and AIH may have a mix of symptoms common to both disorders: Hepatomegaly, jaundice, and elevated liver enzymes are examples of hepatic symptoms. Fatigue, joint discomfort, skin rashes, and fever are examples of systemic symptoms. Anemia, renal impairment, and neuropsychiatric problems are among the further symptoms.
Diagnosis Clinical, serological, and histological results must be carefully considered in order to diagnose AIH and SLE overlap syndrome. Doctors need to distinguish between the characteristics of SLE and AIH and make sure they coexist.
1. **Clinical Evaluation**: Comprehensive history and physical examination to evaluate symptoms like rash, tiredness, and liver problems.

2. **Laboratory Tests**: Liver inflammation is indicated by liver function tests (LFTs).ANA, anti-dsDNA, and liver-specific antibodies such as anti-smooth muscle antibody (SMA) are examples of autoantibody profiles.
3. **Biopsy and Imaging**: – Imaging to evaluate the anatomy of the liver. A liver biopsy is frequently necessary to diagnose AIH and assess liver damage. ### Care and Handling A customized strategy that addresses both hepatic inflammation and systemic autoimmune activity is needed to treat AIH and SLE overlap syndrome.
1. **Immunosuppressive Therapy**: Prednisone and other corticosteroids are frequently used to lower inflammation and suppress the immune system.For long-term care, mycophenolate mofetil or azathioprine may be added.
2. DMARDs (disease-modifying antirheumatic medications):Because of its systemic benefits in SLE involvement, hydroxychloroquine is frequently administered. Non-steroidal anti-inflammatory medications (NSAIDs) are used to treat fever and joint discomfort.If necessary, treat skin rashes with topical or systemic medicines.
3. **Continuous Monitoring and Follow-up**: – Consistent monitoring of systemic symptoms and liver function to modify treatment as necessary.Frequent examinations to identify any negative effects of medication or disease development.
Supportive Care and Lifestyle Lifestyle modifications and supportive therapies can help manage symptoms and enhance quality of life in addition to medical treatment:

**Nutrition and Diet**: A well-balanced diet to lower systemic inflammation and promote liver health. To preserve joint mobility and lessen tiredness, engage in regular, moderate exercise. **Psychological Support**: Support groups or counseling to help manage the emotional strain of having a chronic illness.
## Wrap-up There are particular difficulties in diagnosing and treating systemic lupus erythematosus and autoimmune hepatitis because of their comorbidity. Healthcare providers can successfully control symptoms and enhance patient outcomes by offering tailored therapy based on their comprehension of the intricacies of this overlap syndrome. Making lifestyle changes, actively participating in their treatment plan, and remaining knowledgeable about their disease can all be crucial to a patient’s ability to manage their health. To better understand overlap syndromes and improve patient care in the field of autoimmune disorders, more research and education are needed.

