Why TB Medications Could Harm Your Liver—Expert Analysis
Overview:
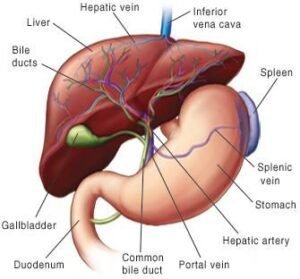
One of the biggest causes of sickness and mortality in the globe is still tuberculosis (TB). Antituberculosis medications have transformed the treatment of tuberculosis, but there is serious worry about their link to liver damage. Effective TB management is hampered by drug-induced liver injury (DILI), which is brought on by these drugs and frequently necessitates close observation and therapy modifications. This article examines the complex relationship between liver damage and antituberculosis medications, emphasizing risk factors, causes, and mitigation techniques.
 Knowing How Antituberculosis Drugs Affect Liver Damage
Knowing How Antituberculosis Drugs Affect Liver Damage
First-line medications such as isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), and ethambutol (EMB) are commonly used in antituberculosis treatment. Although these medications fight Mycobacterium tuberculosis in concert, it is impossible to ignore the possibility of hepatotoxicity. The main causes of liver damage among them are pyrazinamide, isoniazid, and rifampin.
Mechanisms of Reactive Metabolites and Hepatotoxic Metabolic Activation
The liver produces reactive metabolites as a result of the metabolism of isoniazid and rifampin. Hepatocyte damage and oxidative stress can result from these metabolites’ ability to attach to cellular proteins.
Immune-Induced Reactions
Immune-mediated liver damage is triggered by some antituberculosis medications. For example, hapten production from isoniazid metabolism can trigger an immunological reaction against liver cells.
Combined Toxicity
Because isoniazid and rifampin or pyrazinamide have synergistic effects on hepatic enzymes, they can exacerbate liver injury and increase the risk of toxic metabolite buildup.
Risk Factors for Antituberculosis Drug-Related Liver Damage
Genetic and Demographic Factors
Age: Due to a reduced ability for hepatic regeneration, older persons are more vulnerable.
Sex: Compared to men, women may be more susceptible to drug-induced liver damage.
Genetic Variations: The pace of isoniazid metabolism is influenced by variations in the genes that encode enzymes such as N-acetyltransferase-2 (NAT2). Toxic metabolites are more likely to build up in slow acetylators.
Existing Liver Disorders
DILI is more common in patients with chronic liver illnesses, such as non-alcoholic fatty liver disease (NAFLD), hepatitis B, or hepatitis C.
Co-administration of additional medications
Liver damage is more likely to occur when hepatotoxic medicines or alcohol are used concurrently.
Status of Nutrition
The liver’s capacity to metabolize antituberculosis medications might be hampered by malnutrition and nutritional deficits, which can increase toxicity.
Liver Injury’s Clinical Presentation Antituberculosis medications can cause a range of liver damage, from moderate enzyme increases to severe drug-induced acute liver failure (DIALF). Typical signs and symptoms include:
 Weariness and malaise
Weariness and malaise
Feeling queasy and throwing up
Jaundice
Pain in the Upper Right Quadrant
Pale stools with dark urine
Hepatic damage is characterized by elevated levels of liver enzymes such as bilirubin, aspartate aminotransferase, and alanine aminotransferase (ALT).
Methods for Preventing Antituberculosis Drug-Induced Liver Damage Before Treatment
To determine which patients are at risk, do baseline liver function tests (LFTs).
Check for alcohol use patterns and liver conditions that may already exist.
 Monitoring of Therapeutic Drugs
Monitoring of Therapeutic Drugs
Throughout treatment, closely monitor LFTs, particularly in high-risk patients.
If there is severe liver damage, go to second-line medications or modify dosages.
Pharmacogenomic Examination
Find genetic variations in enzymes such as NAT2 to tailor treatment and reduce toxicity.
Supplementary Treatments
To protect liver health, use hepatoprotective substances like silymarin or N-acetylcysteine (NAC).
To maximize hepatic metabolism, make sure you are getting enough nourishment.
Patient Awareness and Education
Inform patients on the need of promptly reporting symptoms and the early warning signals of hepatotoxicity.
When to Stop Therapy or Change It
It is necessary to stop or alter antituberculosis treatment when there is significant liver damage, which is usually indicated by:
elevated ALT or AST readings without symptoms that are five times the upper limit of normal (ULN).
ALT or AST readings that are more than three times the upper limit of normal, accompanied by symptoms like jaundice or stomachache.
Starting with the least hepatotoxic medication, a stepwise desensitization procedure should be followed when reintroducing therapy.
New Research and Prospects for the Future
The creation of less hepatotoxic antituberculosis regimens is being investigated by recent developments in pharmacology. Delamanid and bedaquiline are promising options since they show fewer hepatic adverse effects. Additionally, studies on biomarkers for DILI early identification have the potential to completely transform patient care.
Despite being essential in the treatment of tuberculosis, antituberculosis medications have a considerable risk of liver damage. Optimizing treatment outcomes requires a thorough understanding of risk factors, processes, and preventive interventions. We can lessen the effects of hepatotoxicity and guarantee the effectiveness of TB treatment by emphasizing individualized strategies and close observation. Healthcare Professionals’ Role in Treating
Drug-Induced Liver Injury
In order to prevent and treat liver damage brought on by antituberculosis medications, healthcare professionals are essential. Results can be greatly impacted by a proactive approach to patient care.
Patient Education and Counseling

Unintentional overdoses and treatment interruptions are reduced when patients are taught the value of following recommended dosages and schedules.
Timely reporting and intervention are ensured when liver injury signs, such as black urine or yellowing of the eyes, are communicated clearly.
Multidisciplinary Group Method
Treatment strategies can be improved by pulmonologists, hepatologists, and clinical pharmacists working together, especially for patients who are at high risk.
By including nutritionists in care teams, patients are guaranteed the right nutritional support, which promotes liver healing and general health.
Lifestyle Changes’ Contribution to Risk Mitigation
The risk of liver damage can be increased or decreased by lifestyle choices. Adopting behaviors that promote liver health should be recommended to patients receiving antituberculosis medication.
Steer clear of alcohol and other toxins.
Alcohol raises the risk of severe hepatotoxicity by dramatically increasing the burden on the liver. During treatment, total abstinence is highly advised.
A well-balanced diet
Oxidative stress in liver cells can be lessened by eating a diet high in antioxidant-rich foods such as fruits, vegetables, and whole grains.
Omega-3 fatty acids may lessen inflammation, and a healthy protein diet promotes liver repair.
Sustaining a Healthy Weight
Liver damage can be made worse by obesity. Promoting moderate, consistent physical activity among patients aids in maintaining a healthy weight.
Global Consequences and the Significance of Public Health
Liver damage brought on by antituberculosis medications is a public health issue as well as a clinical one. Low- and middle-income nations are disproportionately affected by TB because they have less access to healthcare, greater rates of malnutrition, and pre-existing liver diseases. To overcome these issues, public health infrastructure must be strengthened.
Accessible Monitoring Tools Are Necessary
Even in environments with limited resources, making liver function testing kits widely accessible can aid in the early detection of liver damage and the avoidance of mortality.
Educating Medical Personnel
In areas where tuberculosis is endemic, healthcare professionals should get ongoing training on identifying and treating DILI.
Programs for Community Awareness
Morbidity and mortality linked to liver injury can be decreased by increasing community awareness of TB therapy, its side effects, and the significance of getting medical attention.
Investigations into Alternative Medicine
With an emphasis on lowering hepatotoxicity, the field of TB treatment is developing. The goal of ongoing research on alternative medications and regimens is to strike a balance between safety and effectiveness.
Systems for Targeted Drug Delivery
Therapeutic delivery methods based on nanotechnology are being investigated to guarantee localized therapeutic action and lessen systemic adverse effects, such as liver damage.
Biological Treatments
A viable substitute with a decreased risk of hepatotoxicity is the use of biologics, such as monoclonal antibodies that target Mycobacterium tuberculosis.
Changes in Pharmacology
One viable approach is to change the chemical makeup of currently available medications to lessen the production of harmful metabolites.
In conclusion
Antituberculosis medications can cause serious liver damage, yet they are extremely helpful in the fight against tuberculosis. Numerous intricate processes are involved in the pathogenesis, including immunological responses, metabolic activation, and synergistic effects. Healthcare professionals can reduce hepatotoxicity and enhance patient outcomes by being aware of the risk factors, following monitoring procedures, and changing lifestyle choices.
Future developments in personalized medicine and medication development could lead to safer treatments, which would lessen the prevalence of liver damage globally. Effective TB treatment and liver health preservation can coexist in harmony with continued research, patient education, and vigilance.