Does Renal Replacement Therapy Really Help in Acute Liver Failure? ♦A Clear-Cut Guide for Nurses & Clinicians
Meta Description
Discover how Renal Replacement Therapy (RRT) supports patients with acute liver failure. Learn its types, benefits, limitations, and nursing care essentials in this easy-to-understand guide for healthcare professionals.
Focus Keywords:
Renal Replacement Therapy, Acute Liver Failure, CRRT in liver failure, Nursing care in liver disease, Hepatorenal syndrome
—
Introduction
Acute Liver Failure (ALF) is one of the most challenging emergencies that healthcare professionals face. It progresses rapidly and can lead to multi-organ failure in a matter of days. One of its most common and serious complications is acute kidney injury (AKI).
To manage this, clinicians often turn to Renal Replacement Therapy (RRT) — a lifesaving method used to support failing kidneys. But does RRT really help in acute liver failure, or does it simply buy time until the liver recovers or a transplant is available?
In this guide, we’ll explore RRT’s role in acute liver failure—what it does, how it helps, and the vital nursing care considerations every healthcare worker should know.
—

Understanding Acute Liver Failure (ALF)
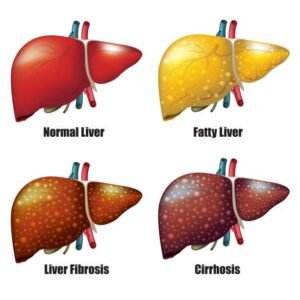
Acute liver failure occurs when the liver suddenly loses its ability to function within days or weeks. This is different from chronic liver disease, where damage happens gradually.
Common Causes of ALF
Viral hepatitis (A, B, or E)
Drug-induced injury (especially paracetamol/acetaminophen overdose)
Autoimmune hepatitis
Ischemic injury
Herbal or toxin exposure
Key Features of ALF
Coagulopathy (INR > 1.5)
Hepatic encephalopathy (confusion, altered sensorium)
Jaundice and fatigue
Multi-organ dysfunction, especially renal failure
—
Why Do Kidneys Fail in Liver Failure?
The liver and kidneys are closely linked. When the liver fails, it causes systemic changes that impair kidney function.
Main Mechanisms
1. Decreased blood flow to kidneys: Systemic vasodilation reduces renal perfusion.
2. Inflammatory injury: Accumulation of toxins and cytokines damages kidney tissue.
3. Oxidative stress: Increases tubular injury.
4. Drug toxicity: Certain liver medications can worsen renal function.
This condition is often called Hepatorenal Syndrome (HRS)—a form of kidney failure secondary to liver dysfunction.
—
What Is Renal Replacement Therapy (RRT)?
Renal Replacement Therapy replaces the blood-filtering function of the kidneys. It removes toxins, controls fluid and electrolytes, and maintains acid-base balance when kidneys stop working.
Types of RRT
1. Intermittent Hemodialysis (IHD)
Sessions last 3–4 hours
Rapid toxin removal but can cause hypotension
Not ideal for unstable ALF patients
2. Continuous Renal Replacement Therapy (CRRT)
Gentle, 24-hour filtration
Maintains hemodynamic stability
Best suited for critically ill ALF patients
3. Sustained Low-Efficiency Dialysis (SLED)
A middle-ground option between IHD and CRRT
Effective in resource-limited ICUs
👉 CRRT is generally the preferred option in acute liver failure due to its gentle and continuous nature.
—
How RRT Helps in Acute Liver Failure
While RRT cannot heal the liver, it supports vital functions and prevents complications.
1. Ammonia Clearance
High ammonia causes hepatic encephalopathy and cerebral edema.
CRRT continuously removes ammonia, improving mental status.
2. Fluid Balance
ALF patients retain fluid due to low albumin and kidney dysfunction.
RRT helps remove excess fluid safely, reducing pulmonary and cerebral edema.
3. Electrolyte Management
Corrects sodium, potassium, and calcium imbalances.
Prevents arrhythmias and muscle weakness.
4. Acid-Base Stabilization
Restores normal blood pH levels.
Supports cardiac and metabolic function.
5. Removal of Inflammatory Mediators
CRRT filters out cytokines and endotoxins, limiting systemic inflammation.
6. Bridge to Liver Transplant
RRT keeps patients stable until they receive a liver transplant.
Improves pre-transplant condition and post-operative outcomes.
—
Limitations of RRT in Liver Failure
RRT provides support but not a cure. Nurses and clinicians must understand its boundaries.
❌ Does not restore liver function
⚠️ Risk of hypotension during fluid removal
⚠️ Bleeding risk due to coagulopathy
⚠️ Nutrient loss (amino acids, vitamins)
💸 High cost and equipment needs in continuous modes
Hence, RRT is a supportive therapy, not a replacement for liver function.
—
When to Start RRT in Acute Liver Failure
Early initiation improves outcomes. Start RRT when the patient develops:
Serum creatinine > 2 mg/dL
Fluid overload unresponsive to diuretics
Severe hyperammonemia
Metabolic acidosis (pH < 7.1)
Electrolyte imbalance (e.g., hyperkalemia)
Clinical judgment and team discussions are essential before initiation.
—
Nursing Responsibilities During RRT in ALF
Nurses play a central role in managing patients undergoing RRT. Their vigilance and assessment skills directly impact survival.
1. Hemodynamic Monitoring
Continuous BP, HR, and CVP monitoring
Report hypotension or shock immediately
2. Neurological Observations
Assess for changes in consciousness
Watch for worsening encephalopathy
3. Fluid Balance Charting
Record all inputs and outputs accurately
Adjust therapy to prevent dehydration or overload
4. Infection Control
Maintain strict asepsis during catheter care
Observe for bleeding or leakage at access sites
5. Lab Monitoring
Check ammonia, urea, creatinine, and electrolytes
Review ABG and liver function trends regularly
6. Nutritional Support
Collaborate with dietitians for high-calorie, controlled-protein diets
Replace vitamins lost during dialysis
7. Team Communication
Update the multidisciplinary team on therapy response
Coordinate with the transplant team if indicated
—
What Research Says About RRT in ALF
Studies show early CRRT improves ammonia clearance and neurological recovery.
Continuous therapy maintains better hemodynamic stability than intermittent dialysis.
RRT improves short-term survival, especially in patients awaiting liver transplant.
However, the final outcome depends on liver recovery or transplant availability.
—
Future Perspective: Combined Liver-Kidney Support
Emerging technologies are combining RRT with artificial liver support systems to provide both hepatic and renal detoxification.
Examples Include:
MARS (Molecular Adsorbent Recirculating System)
Prometheus System
SPAD (Single Pass Albumin Dialysis)
These systems remove protein-bound toxins that traditional RRT cannot. Though still under study, they show promise for the future of multi-organ support.
—
Conclusion
Renal Replacement Therapy is a lifesaving support system for patients with acute liver failure and renal dysfunction. It does not cure liver disease, but it buys valuable time—allowing other organs to recover and increasing survival chances until liver regeneration or transplantation.
For nurses and clinicians, early detection, timely initiation, and careful monitoring during RRT are vital to improving patient outcomes.
In critical care, RRT is not just a therapy—it’s a bridge to hope.